So some good news – I came off IV’s yesterday. It looks like I will be free to enjoy the rest of my summer.
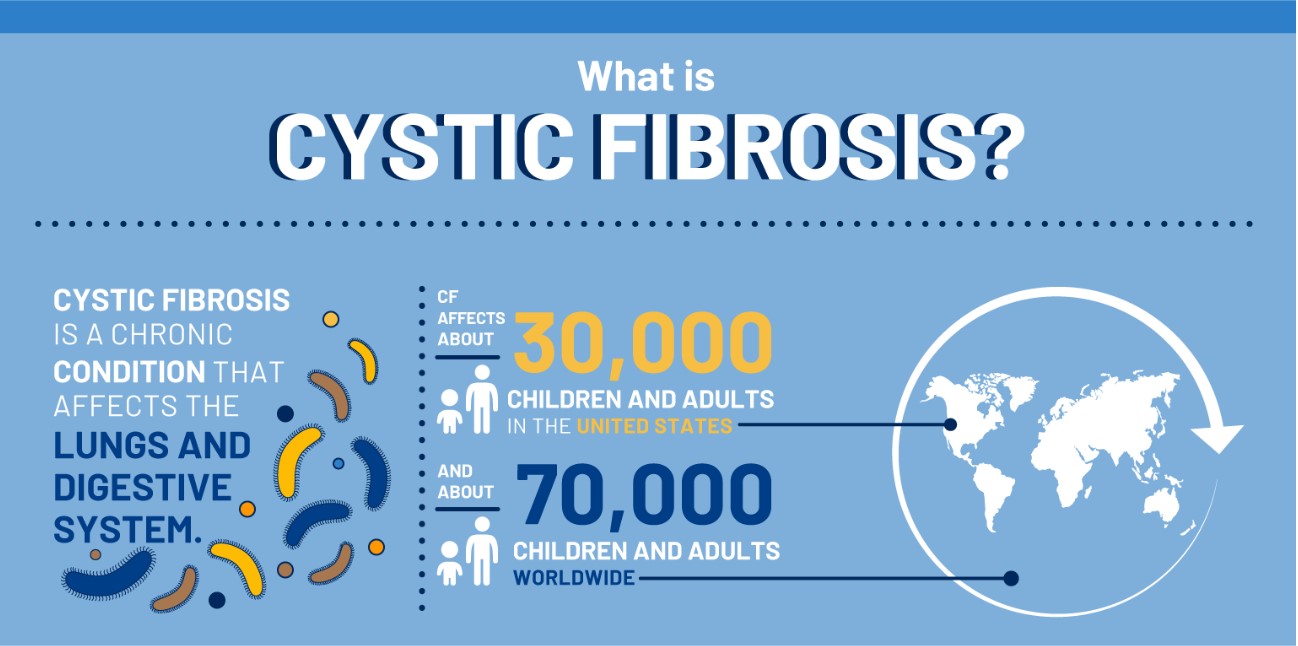
Coincidentally, I’ve gotten a few questions about how I am able to manage my time while I’m on IV. So I figured we can tackle that topic in a blog post today. Remember, though, IV treatments are a very serious thing. It’s important to make sure you are always on the same page with your doctor and homecare team. Don’t go running around saying, “oh Gunnar Esiason said this is what he does when he’s on IV, so I can do it too!” I’ve had at least two-dozen courses of IV antibiotics over the past 26 years, so I’ve got a good bit of experience with this. Ultimately you need to decide with your care team if homecare is right for you, and if it isn’t that’s fine too!
First off, I am on team PICC line over Port (I can get into that argument at a later date, I just happen to have really friendly veins), and I always go the homecare route when I can. I think I’ve proven to my care team that I am responsible enough to manage my health outside the hospital, even when I am sick (with the help of doctor mom). If I am unable to fulfill the requirements of a course of treatment, I never hesitate to go inpatient. Luckily it has been awhile since I’ve needed to stay inpatient.
When I need to go on IV, and I’m in the clear to use homecare, I use a local hospital’s IR (Interventional Radiology) unit to get the line placed. My CF clinic is at a major hospital in NYC, Columbia Presbyterian, and it can be a nightmare to get simple things done in that setting. I’ve found that it has been stress reducer to use a hospital in my hometown – basically 5 minutes from where I live. The smaller hospital usually leads to less of a wait time, and a quicker overall procedure. My CF team in NYC actually recommended this path to me for those reasons. It’s also easier to get the IV started in a timely manner, meaning a quicker jump to antibiotics and, hopefully, path to feeling better much sooner. Also, credit where credit is due, the IR team at my local hospital, North Shore University Hospital is absolutely amazing – they do a fantastic job for people with CF.
When I’m on homecare I live for the Eclipse balls. They are self-pumping IV bags. I never use an IV pole. I demand mobility. I figure people with CF are sick so often (at least in my case, I find myself not feeling well more often than I’d like), so I like to return to normal life as soon as I can. The Eclipse balls give me that opportunity. The homecare company certified my mom and I to reconstitute meds in an Eclipse ball rather than an IV bag for the certain medications with short shelf lives (the time in which the medication lasts from the time it has been reconstituted). I’ll admit that process is a complete pain in the ass, and is probably something that people without a good deal of IV experience shouldn’t attempt, but it certainly helps with my mobility. An extra note here – I’ve come to learn that Health Canada doesn’t always offer Eclipse Balls to patients for whatever reason, and makes people rely on the IV pole. If you’re Canadian and you’ve been able to go mobile while on IV, help your fellow countrymen out in the comments below.

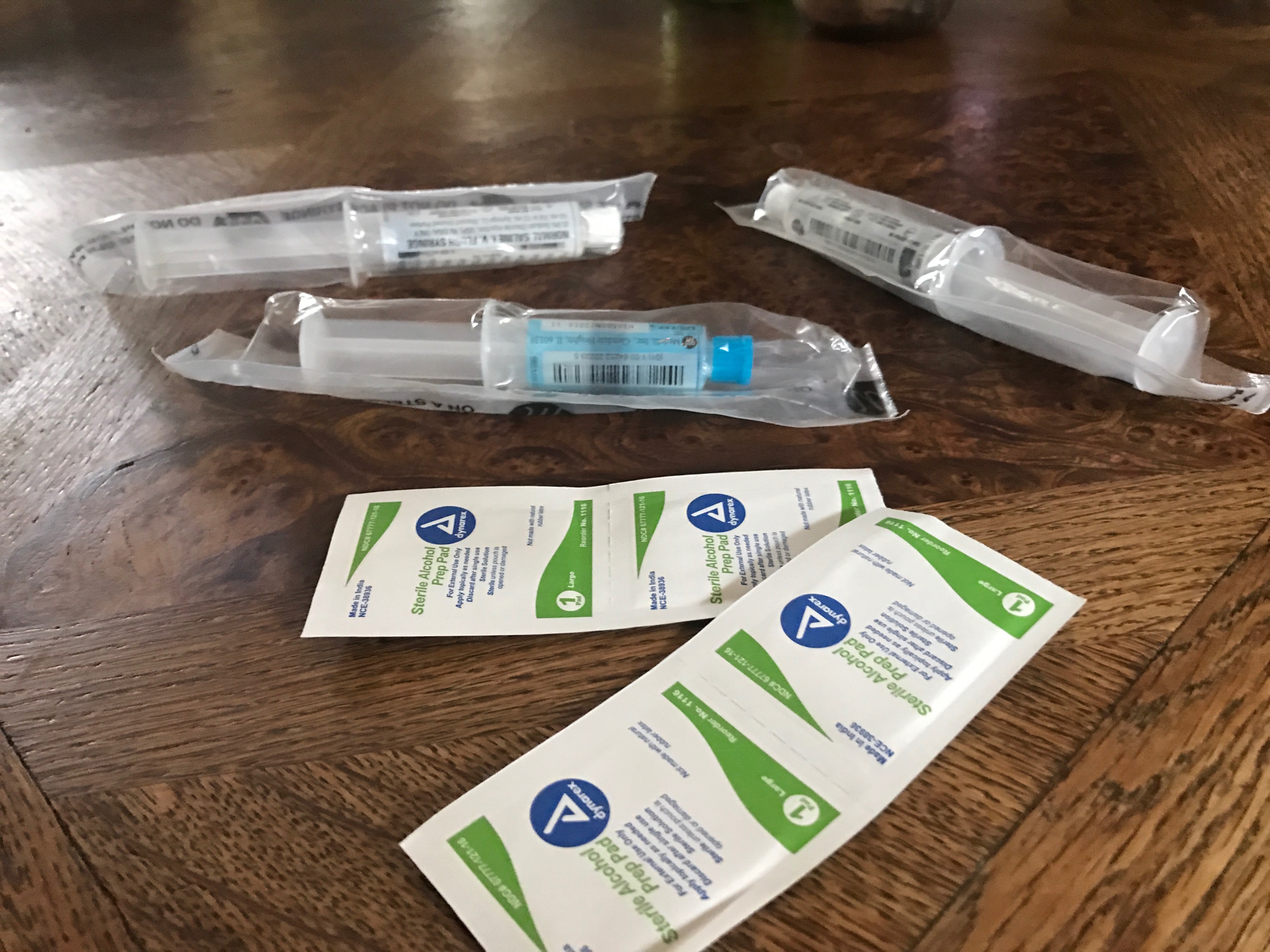
This is what the Eclipse Balls look like. This one is a little bigger than others – 500ml/2hr ball – it is filled with IV hydration. One downside is that the drip rate and dose aren’t flexible like a traditional pump – so it may not work for everyone.
My parents never hesitated to put me back in school a few days after having an IV placed. My general rule has always been to take as much time as needed to get back on my feet then return to the swing of things with any needed adjustments. When I was middle school and high school, my mom or dad would come by the school around lunch time, start the med infusion, then return when the drug was due to end. The Eclipse balls played a large role in this little plan, because I could return to class or whatever activity with the IV bag in my pocket. My parents made the school and my teachers aware of our little scheme. In a way, the school loved it because I wasn’t missing classwork. As far as anyone knew, I was taking an extended bathroom break. By the time I was in college and had learned how to run the IV’s myself with an extension line, I would just excuse myself from class, start the IV in an empty classroom, then return to my ongoing class. I always made sure my professors or teachers at any level were aware of what was going on. Any person with a heart will understand….
I’ve never shied away from light exercise while on IV either. Once my body is back to a place where I think it’s okay to be up and moving, I try to help the treatment with exercise. When I was in high school, I once was incredibly sick and needed IV treatment during my football season. I was raised to believe that missing practice is never acceptable, and is, in fact, one of my principles of life, so I consulted the necessary people in my life. My doctors, family, football coaches and I came up with a plan that would allow me to continue light workouts while on IV. Obviously football is a contact sports, so I wasn’t out there tackling or participating in hard hitting drills, I just managed my cardio conditioning, as well as throwing (I was a quarterback), footwork and anything else that my doctors and coaches deemed appropriate. These days, one of my many jobs is to coach high school ice hockey. I’m a head coach, and since I believe it is unacceptable to miss a day at the rink, I schedule my IV’s around my ice-time whenever possible. There have be a few instances when I’ve gotten an IV placed at the local hospital in the morning, met with the homecare company, then headed over to the rink for practice. I doubt my players have ever noticed anything was amiss.
I’ve actually traveled while on IV as well. I mentioned in a blog post last week that I took my homecare IV’s to my friend’s wedding in Chicago. In college I also went on spring break my senior year while on IV. My doctors know that I am a responsible patient, so they gave me the green light in both cases. Traveling is not easy with IV’s. It requires a lot of patience, planning and teamwork. The first time I did it, my family got some advice from the homecare company and my care team about how to plan for all contingencies, for example always having an Epi-Pen. I ended up packing more IV hydration than I’d normally need as well as an extra day’s worth of medications in the event an Eclipse Ball had a malfunction (shit happens… things don’t always work). I also had a prepared statement for airport security. It’s not uncommon for people to travel while on IV (CF or whatever else). My advice here would be to make sure that you, the parent, or you, the patient, have enough of a comfort level when it comes to using the IV system. You need to be able to troubleshoot and you have to have a phone number to call if the shit hits the fan and you need an answer immediately. It’s also critical to discuss the plan with your doctor and homecare company – your health needs to be in a place where it is safe for you to travel. Most recently when I went to my buddy’s wedding in Chicago, packing was a major undertaking. My girlfriend and mom played a big role there because I was feeling like shit in the moment. So big thanks to them for helping when I needed it.

I don’t think this totally does the packing job justice. This is just a fraction of the gear I traveled with to my friend’s wedding (minus the Gatorades and water – kind of a weird product placement there), and doesn’t include my Vest or nebulized meds.
Develop a great relationship with your homecare nurse. Nurses are a patient’s lifeline when it comes to dealing with different medical situations that fall out of the ordinary, like IV’s. The nurse is often the first line of defense against an unforeseen situation. I always like to have the same nurse when I go on IV, because it helps fight off some stress or anxiety that comes with being sick. I can’t say enough about my nurse, she’s absolutely amazing.
Finally, the last piece of advice here is something that a homecare nurse once gave to me, don’t let you IV rule your life. The best way to transition from a healthy patient, to a patient onto IV, and finally back to a healthy patient is by creating a schedule that works for you. Often times there is a late night infusion coupled with an early morning infusion. It’s okay to reach out for help with your IV. I’m 26 and I lean heavily on my mom when I get sick. My mom and I always split the work when I initially get sick – for example I’ll do the late night infusion and she will help with my early morning one. The patient’s lifestyle during treatment is as much of a factor in returning to health, as is the actual treatment. My mom is always up to the challenge of helping (I think it’s because I get to be her baby boy again). My dad lost his privileges in this department after he once pulled a cap off by accident. Eye roll. I also have a few friends who have very basic training with using my IV, and my girlfriend is constantly all up in my shit about one day learning how to use it – one day she’ll get to learn. The only way you’re going to get better is by using the IV correctly and in an effective way. Antibiotics are incredibly toxic and almost always drain the body. You need to be able to rest, hydrate and focus on returning to health.
What are your home IV strategies?