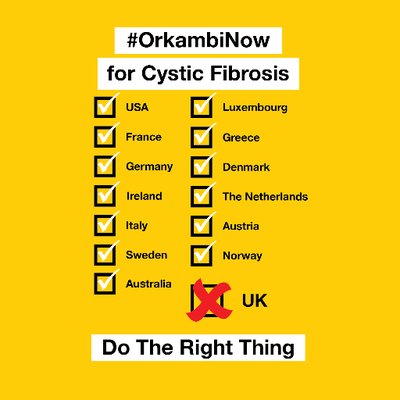
Amy is back with part two of her discussion concerning access for CFTR Modulators. Today we take a look at what’s preventing people with CF from gaining access to Orkambi in the United Kingdom
I’m a DF508 heterozygote and therefore don’t have a CFTR modulator that will work for me (hopefully late 2019 it will be my turn). Of course I wish I could benefit from a CFTR modulator right now, but I know my time will come – and in the meantime, I get so much joy out of seeing others in the CF community benefiting from existing drugs. In fact, one of my dear friends just started Symdeko TODAY and I’m at the edge of my seat waiting to hear how he feels.
That being said, I can’t fathom what it must feel like to know there is a CFTR modulator out there that would work for my mutations, but to not have access to it.
On July 2, 2015 the American FDA approved Orkambi for cystic fibrosis patients 12 and older with two copies of DF508 – the first medication ever to treat the underlying cause (defective protein) of CF for those with the most common combination of mutations in the world. It’s October 2018, and Orkambi is not widely available in the UK (except for a few compassionate care cases) – and like everyone else, I’m devastated about this. It’s simply not right.
Why is it that UK CFer’s don’t have access to this medication for 3+ years that has helped so many in the US?
Simply put, NICE (The National Institute for Health and Care Excellence in the UK) states that Orkambi isn’t cost effective:
“ The committee concluded that, even without including any of its preferred assumptions, the estimated incremental cost-effectiveness ratios (ICERs) were considerably higher than what is normally considered a cost-effective use of NHS resources.”
This makes my stomach churn. There is a single entity in the UK – that doesn’t seem to have accountability to anyone – that gets to decide the monetary value for a person’s health. I’m not OK with this for anyone in our CF community, and you shouldn’t be either.
To be crystal clear: I’m not bashing the UK’s healthcare system. I’m not saying that the US’s healthcare system is perfect, or without fault, or ideal. I’m simply examining the current facts: Orkambi hasn’t been available in the UK for 3 years and 3 months.
Lack of Orkambi Efficacy Is A Smokescreen
The truth is yes, not everyone does amazingly well on Orkambi; no one does amazingly well on any drug. No drug is a panacea. However, Orkambi has helped quite a number of people with CF. And the terms “help” and “do well” can be misleading – sometimes CF isn’t about improving FEV1. It can be about reducing FEV1 decline, reducing exacerbations, hospitalizations, increasing beta cell activity or improving quality of life. It’s incredibly narrow minded to think that a drug’s only benefit is simply FEV1 increase – CF is about so much more.
As we discussed in the last article, , Orkambi cuts exacerbation rates in half in CF patients. What’s more, a 96 week study of patients on Orkambi and placebo showed that those on Orkambi reduced the annual rate of lung function decline by ~42%. And you’re telling me it’s OK that the UK doesn’t pay for Orkambi because it doesn’t really work that well? I would do anything to reduce my annual FEV1 decline by 42%!
Orkambi “may modify the progression of CF lung disease by treating its underlying cause,” said Michael W. Konstan, M.D., Vice Dean for Translational Research at Case Western Reserve University School of Medicine and Vice Chair for Clinical Research at University Hospitals Rainbow Babies & Children’s Hospital.
NICE is getting in the way of preventing the progression of CF lung disease. This. Is. An. Outrage.
Let’s pretend for a second that NICE’s smokescreen is correct (which it isn’t) and Orkambi doesn’t work very well anyway- why doesn’t the NHS allow DDF508 patients to try Orkambi to see for themselves? Surely patients would discontinue the drug and the NHS wouldn’t have much expenditure if this scenario played out, right?
I fear that the NHS has duped some in the UK CF community in to believing that Orkambi will have little to no impact on a CFer’s health. This could serve to direct outrage towards Vertex, instead of where it should be – towards NICE and the NHS.
Cost
I’ve heard some in our community state that Orkambi’s price is OUTRAGEOUS at £104,000 per patient per year before discounts. Is it? Then why are so many other countries across the world providing access to their patients? Perhaps other countries realize that because – as I spoke about in my previous article – in order to develop breakthrough medications for the orphan diseases, the small populations require a higher drug price.
“But those countries that offer Orkambi to their CF patients are probably paying less than the list price of Orkambi and are instead paying a negotiated rate”, I hear in reply. Of course every country is paying a negotiated rate – no one pays the list price of the drug. The UK of course wouldn’t pay list price either! Private insurance companies in the US don’t pay list price; neither does the US federal government.
“In the latest [2018] meeting, we made the best offer in the world to NHS England,” Vertex said. The UK has a history of playing these games, not just in cystic fibrosis care.
“Thousands of NHS cancer patients in the UK are missing out on innovative treatments available in countries of comparable wealth partly because of a failure by medicines [sic] regulators to negotiate with the pharmaceutical industry on the price of drugs, charities have said.”
I see a pattern.
A 2016 report published by Breast Cancer Now and Prostate Cancer UK points out NICE has not approved a single new breast cancer drug for routine use in the NHS in the last seven years. “We know cancer outcomes are worse than in some other countries in Europe and part of that is going to be access to treatment,” said Sally Greenbrook, policy manager at Breast Cancer Now.
“They are placing a lower value on the life of a CF patient than other countries around the world,” states Vertex. Given the NHS’ pattern of holding back innovative medications to UK citizens – not just in CF but in other disease states – it’s hard to not agree with this statement.
Dear NHS: you have to pay for innovation just like everyone else. I’m confused as to why you feel you’re different than the rest of the world, while making CF patients suffer unnecessarily the past 3 years.
“Buuuuuuuuut AMY! The UK has such a high % of its population with CF – it’s more of a burden to the UK than other countries.”
No it’s not –the UK has 10,400 CFer’s with a total population of 65.64 million – that’s 0.016% of the population – 0.0.10% in the US. That’s a smokescreen!
We have to be very honest and real about where the NHS’ money is going. The cost of diabetes to the NHS an estimated £14 billion pounds [$18.5 billion US] is spent a year on treating diabetes and its complications (10% of costs are related to Type 1 diabetes).
With approximately 4,856 DDF508 patients in UK, and a cost of £104,000 per year per patient prior to discounts, that’s a cost of £505 million a year for a disease that can’t be prevented or reversed by diet and exercise.
Did you catch that? The NHS’ annual cost for Orkambi for all DDF508 patients would be 3.6% of the NHS’ annual cost of treating diabetes.
In 2017, the UK spent £140 billion on healthcare. £505 million on Orkambi would represent 0.36% of the annual budget! 0.36% is a rounding error.
So let’s review: the efficacy of Orkambi is very well documented, and cost is negligible for the UK healthcare system, why in the world doesn’t every UK CF patient have access to Orkambi? Why does the UK have a pattern of withholding innovative treatments across various disease states? There is no excuse.
Moving forward, when Symdeko (Symkevi) receives marketing authorization by the European Commission, and hopefully next year when triple combo Phase III studies are finished, I fear there will be further delays in access to CF patients in the UK.
2018 should be the best time to be alive with CF for everyone – not just part of our population lucky enough to live within certain political borders. To my UK CF brothers and sisters – Fight On!
The views expressed on any guest column [Drug Development Wednesday], are that of guest contributors, and not necessarily those of Gunnar Esiason or the Boomer Esiason Foundation. Nothing in guest columns should be considered medical advice; such advice can only be given by a physician who is experienced with cystic fibrosis. The Boomer Esiason Foundation, Gunnar Esiason, and guests cannot be held responsible for any damage which may result from using the information on this website without the permission of your medical doctor.