In no small way has the triple combo completely changed my life. The first few weeks of the study were some of the most powerful of my life. My lung function seemingly skyrocketed over night, I suddenly felt like I had more energy than an Olympic athlete in the prime of his career, and the nagging cough that we all know vanished. In fact, it’s almost hard to remember what life was like before the study. In those days I was largely living day to day or month to month between needing to use IV’s, trying different antibiotics or enduring abrupt pauses in my life.
Since it was broadcast to the world that I was a trial participant (I was given the green light to discuss participation following the FDA approval), I have gotten a seemingly endless line of questions about what it’s like to be on the drug, so we will answer a few of the most common below! As you read, though, don’t take my word for medical advice. If there is one commonality between all of the modulators that are on the market, it’s that they all affect everyone a little differently. It is absolutely critical that you discuss the pros and cons of Trikafta (and any medication for that matter) with your care team, and NOT use the Internet, and certainly not my blog, as the end all, be all of medical decisions.
Did your PFT’s go up?
YES! My PFT’s basically exploded. While I am not going to give you specifics here (if you browse my blog all the way back to the beginning you’ll see that I never share PFT scores), I will say that according to some respiratory disease gauges, I improved from severe respiratory illness to moderate respiratory illness. My results were largely in line with the published results.
Did it really work almost immediately?
A lot of news sources quoting my experience have been hanging on the idea that the drug started working very, very quickly. Could I actually tell that it was working right away? You bet your ass I could. About 10-12 hours after starting in the trial my cough increased dramatically, and the feeling of the mucus started to change. The first few days on drug, mucus basically poured out of every opening in my body, and then it suddenly stopped. In the midst of it all, I had some weird unexplained feeling in my stomach/GI area, and my o2 sats climbed to 100% (a number I had never previously seen when I tested on multiple different fingers). It all just seemed like way too much of a coincidence.
Is it easier to exercise?
This tweet post from June, 2018 should speak for itself given the new context…
Were you able to stop doing treatments?
No, not exactly. Trikafta is not a cure, and it is important that if you end up using it, you don’t expect it to be a cure. I have bronchiectasis in my lungs, and that’s not going way, nor is the pseudomonas (at least for now! We can always hope, right?). That being said, my treatment burden has significantly decreased. I do between 35 and 40% fewer treatments now than I did before starting the trial. I still use inhaled antibiotics every other month, but that’s a huge decrease from what I used to do. I used to alternate antibiotics every month, but now I only rotate one. That alone has made a huge difference in my quality of life.
No one has asked this, but this is what the follow up question should be: Do you feel comfortable decreasing your treatment load?
Initially I did not. It wasn’t until about 8-12ish months into the study (after I had rolled into open-label) that I started to decrease the treatment burden, and I did it very slowly. I am still not entirely comfortable with the decreased treatment burden, mostly because my treatments kept me alive for all those years. I have a great deal of respect for what my treatments can do for me, and how they’re able to do it, so it’s been a hard thing to wrap my head around. It has been our (our = the doctor + patient shared decision-making game) best guess about what to withhold and when. I know my quality of life has improved significantly since I spend less time strapped to a nebulizer, but I monitor changes in my health very closely since I have fewer treatments in my routine. If I sense the slightest bit of a cold coming on, I snap right back into full treatment mode. One of the most fascinating things about all of this is that we really don’t know how to reduce treatment burden, which is why the CFF is funding SIMPLIFY, an observational study designed to figure out how to reduce treatment burden for people on modulators. I am excited to learn the results of that… if you want more info, ask your care team. It’s been a topic of discussion at the North American Cystic Fibrosis Conference this year.
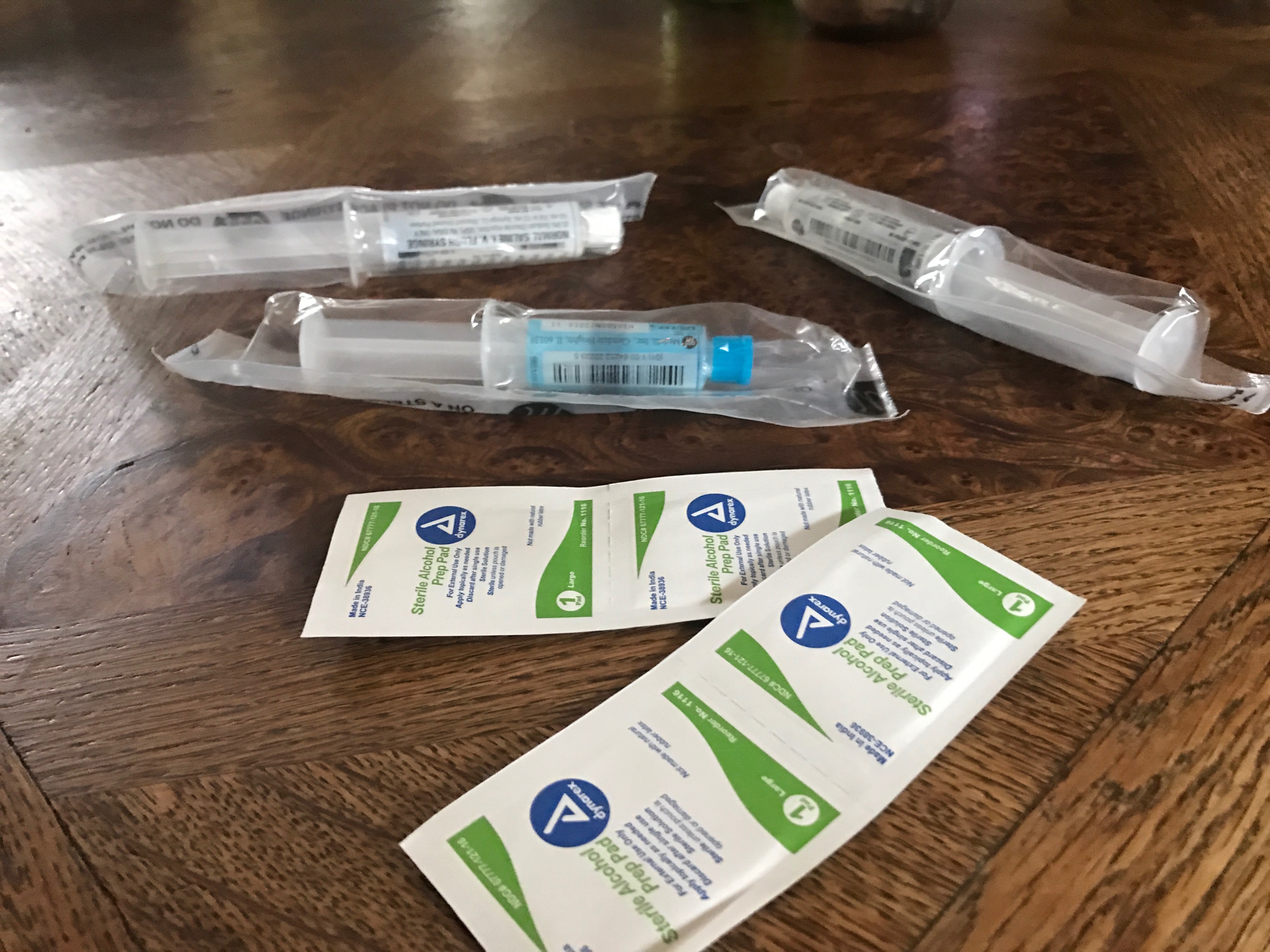
Do you still need to go on IV’s?
Yes. I know it sucks, but while modulators have been shown to reduce some of the bacterial load, after all the lungs kind of work normally, they do not have antimicrobial properties. I still deal with significant drug resistance – something I consider to be one the major hurdles standing between us and a cure – which really really sucks, but I will say I do get a bigger bang for my buck with IV’s. I also use them less frequently. Prior to enrolling in the trial, I had been averaging 3-5 courses of IV’s PER YAER (yeah… I know), but when I started the trial, I went an entire year without needing IV’s. When I finally went on IV it was mostly just to treat that MDR pseudomonas – it’s not the kind of thing we were comfortable with leaving untreated. When I say a bigger bang for my buck, I mean it, too. I have used IV’s twice since starting the triple combo, and each time I do, my PFT ends up flying past my baseline. I have no idea why that happens, and I’m not going to start to guess, rather I’ll wait for the results from the PROMISE study to come out (ask your doctor about that one, too!).
What’s the strangest difference?
The clubbing in my fingers has improved. It is super bizarre. I still have clubbing, but it’s not nearly as severe as it was. About 6-8 months ago, my mom was looking at me, and froze in her tracks. She grabbed my fingers and shouted, “your clubbing! It’s getting better!” Then my dad came in a looked at my fingers and agreed. Darcy then looked later, and she also agreed, and then so did my doctor at the next study visit. Of all things to improve….
Have you gained weight, and do you still need your feeding tube?
Yes, to both. Remember, this isn’t a cure. I have put on some weight, but no I’m not getting fat. To be honest, I don’t love eating, it’s just never been fun. I’m sure Darcy would give you some cognitive health-based explanation as to why I feel that way as it relates to my CF, but I just don’t love eating. On the other hand, I DO love my feeding tube, so yes, I still use it. No, I haven’t been funneling beers through it at B-school.
Has your mental health been affected?
I think everyone who knows me well would tell you that I am the happiest that I have been in a long, long time. They aren’t wrong. I wake up every day in Hanover, New Hampshire seemingly unable to believe that I have made it here considering where I was a few years ago. I have the privilege of living with the woman whom I love and my dog, and I have to opportunity, largely because of this medication, to think about my future, family planning, and, gasp, retirement planning. There isn’t a day that goes by that I don’t think about all that went into this drug… The countless fundraising events, the billions poured into research, the thousands of people with CF who came and went, the man-hours put in by volunteers, researchers, and everyone else in between, and where my life was compared to where it is now.
I cried happy tears first time I played hockey after starting the drug. It was the first time in my entire life when I didn’t have to come off the ice early because I was coughing or got lightheaded. The rush of the air against my face as I carried the puck down the ice that day in 2018 was one of those moments I will never forget as long as I live.
My time in the trial is at the end, and it feels somewhat bittersweet. The trial visits have been so frequently over the past several months that it’s like I am moving on from a huge part of my life. I hope that’s how everyone else in the CF world feels, too. We’ve had a huge success, and now we need to move on to the next one.
I am already on the hunt for a new trial… Remember, it’s up to all of us to advance the science towards an eventual cure for cystic fibrosis. We aren’t done yet!
I am SO excited for access to extend to the rest of our community now that the FDA has seen what it could do for us, and I cannot wait until testimonials start pouring in from other patients in the coming days and weeks. This is an incredibly exciting time, and it makes me so so so so happy!
Nothing on GunnarEsiason.com should be considered medical advice. Such advice can only be given by a board certified physician who is experienced with cystic fibrosis. The contributors on these blogs and podcasts cannot be held responsible for any damage which may result from using the information on this blog/podcast without permission of their medical doctor.