This past weekend I was honored to deliver the 2019 St. Louis University School of Medicine Pre-Commencement address. My very first pediatric doctor at Cincinnati Children’s Hospital, Robert Wilmott MD, is now the acting dean at the SLU School of Medicine and extended the invite to me not long ago. I so very much appreciate how progressive the School of Medicine is to allow a patient to deliver such an address, and my hope is that more people living with cystic fibrosis, or any other condition, are given similar opportunities in the future. Below is my address, and also the recording of it, too!
My part begins at 21 minutes.
Thank you Dr. Wilmott! And of course, thank you to the administration for inviting me to speak here today.
To the St. Louis University School of Medicine Class of 2019, allow me to be one of the first to say congratulations… and more importantly, welcome to the team!
Following graduation, you will carry out the Jesuit tradition of being men and women for others. In doing so, you will be teaming up with patients on their journeys to better health.
You and your patients will play an equal role in the pursuit of common goals.
I stand in front of you embodying the complex medical cases that all of you will face in your careers. I live with multidrug resistant bacteria in my lungs, I am pancreatic insufficient and require a feeding tube, and I am a clinical trial participant. All of that is because a genetic defect causes a certain protein to act inappropriately in my bronchial epithelial cells. More commonly, we call my case, cystic fibrosis. I am one of about 35,000 Americans living with what is otherwise known as the most common fatal genetic illness.
For the friends and family in here who have no idea what I just said, sometimes I have a hell of a time trying to breathe, and other times my poop looks super weird.
It has also been said, but I have to say, not confirmed, that I own the fastest beer funnel time in the history of Boston College – and it was only because I did it through my feeding tube.
With all of that being said, it is now time for a room full of doctors to listen to a patient.
The story of cystic fibrosis is one of the most transformative in medicine. Back in the early 90s when Dr. Wilmont was my doctor, and I, embarrassingly enough was deathly afraid of blood pressure cuffs and thermometers, cystic fibrosis was known as a childhood illness with few patients surviving into adulthood. Now, all of these years later, we are on the precipice of correcting the protein dysfunction at the heart of the condition, and we expect patients to have the opportunity to live long, successful lives. Yes, cystic fibrosis will likely remain a killer for years to come since we have only figured out one piece of the puzzle, but now all of us living with the condition have the opportunity to survive.
All told, I have close to three decades of experience living, breathing and succeeding inside our healthcare system. I have kicked more residents out of my hospital room than I care to count, I have argued defiantly with medical recommendations, and I have had to say, “no I refuse,” far too many times.
BUT… I have also met some of the most brilliant physicians the world has ever known. When I was in Boston I spent time as a patient at Boston Children’s Hospital. My pulmonologist, Dr. Craig Gerard, during one consult, used words that I didn’t even know existed in the dictionary to describe my then present condition.
During the next appointment, though, he refused to allow me to skip out on a college spring break trip because I had developed a pulmonary exacerbation. As he put it,
He saw me as a person, and then as a patient.
More than 20 years ago, at Cincinnati Children’s Hospital, Dr. Wilmott provided the care and comfort my parents needed following my cystic fibrosis diagnosis. He gave them the confidence to know that everything would be “okay.”
At the beginning of last year, my pulmonologist, Dr. Emily DiMango, at Columbia University Medical Center in New York said,
So, what sets them apart from other care providers I have worked with? They value my personal and subjective patient experiences. Today, I demand that my care providers see my more than quarter of a century worth experience in cystic fibrosis as a tangible resource when we develop treatment plans.
Listen to your patients!
As you move through your careers in medicine, just about all of you will have the privilege of participating in some of the most important moments of a person’s life. Good or bad, these are the moments that will be remembered. You might have to be the physician who has to deliver the worst news someone could ever imagine.
You will have to learn how to say, “I’m sorry, the treatment isn’t working.”
You might have to tell a man in his 20’s, “The cancer is spreading and we are running out of options.”
You might even be the one who has to deliver a cystic fibrosis diagnosis to an unsuspecting family.
I have been on the receiving end of some very tough conversations myself, “Gunnar, I’m sorry but it looks like the bacteria is now fully resistant to that antibiotic.”
It never gets any easier, but somehow, I am able to find confidence in my physicians in those moments. I challenge you to discover a novel way to inspire your patients in the worst of times. You will have to find the line between empathy, medical literature and common sense. It will be hard, but all of you wouldn’t sitting here today if you were not ripe for the challenge.
On the other side of things, you might be the physician who gets to be there for the very best moment of someone’s life.
Maybe you get to tell the mother of two that she is cancer free!
You could be the surgeon who tells a child’s parents, “The transplant was a success!”
Or maybe you’re the one who gets to tell an expecting mother, who is having pregnancy complications, that she is responding to the treatment.
You may see 15 or 20 patients in a day, and maybe 1200 patients in a year. For some of those people lying in the hospital bed or sitting across from your desk, you may be one of the most memorable people in their entire lives. You may be the person they interact with on the very worst day or the very best day of their lives. They may remember your voice when you delivered good or bad news fifty years later.
Just like I remember the recovery room staffer who told me I could funnel a beer through my feeding tube! Regardless of the anesthetic haze I was in, it was a conversation I will remember forever.
That is the power you have as doctor, and I especially want you to remember it during your residencies, and then wherever you are as a future leader. It is going to feel like you are pulled in a thousand different directions, but you have to find a way to prioritize patient interaction. You will be remembered for how you handle specific conversations with your patients. It is your responsibility to inspire confidence and trust as you tackle complex cases within an already challenging healthcare landscape.
It is an exciting time to be a physician. There are countless obstacles ahead of you, and more than enough opportunity to overcome them. Believe it or not, challenges and obstacles are good things! They make sure we are adaptive and goal oriented.
All of you in the class of 2019 are here today because you are some of the most goal-oriented, ambitious people in the country! I hope you and your families take pride in that.
What I want you to know is that I am alive today because I, along with the millions of Americans living with a rare disease, am also one of the most goal-oriented people you will ever find, and it is a trait that all of us share with all of you. Patients and doctors are unified in the quest for better health, wellness and success. The relationship begins at the point where common goals between patients and providers are established.
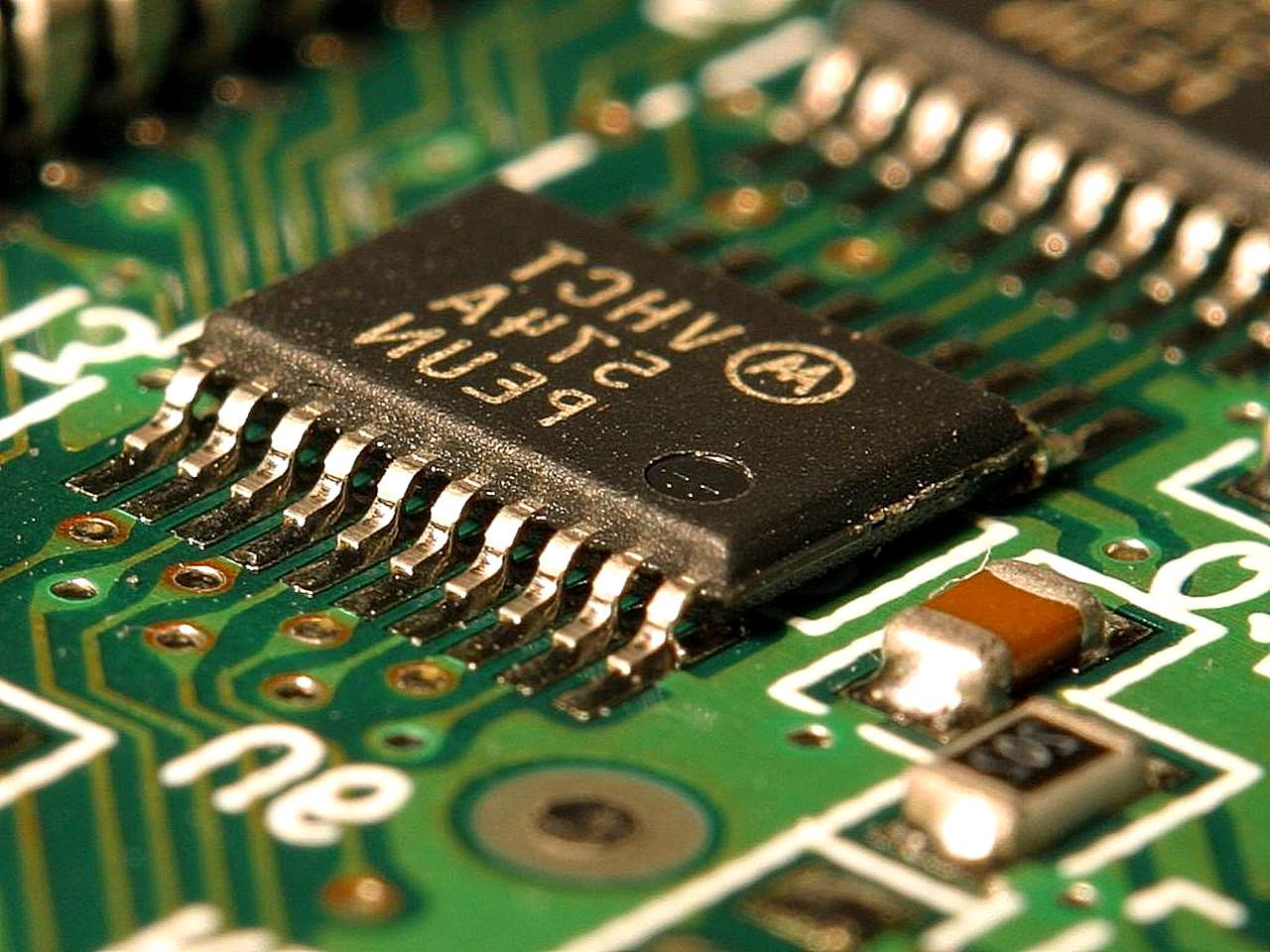
One of the challenges you will face happens to be the single greatest threat in front of humanity – the rise of antimicrobial resistance. Whether you are going into orthopedics, pediatric surgery, oncology, infectious disease, dermatology or anything in between, the odds are quite good you will run into a person facing an antibiotic resistant infection. In fact, not only am I one of those people, but also the CDC tells us that at least 2 million people in the United States get such an infection each year.
It is an enormous problem, and I can tell you from experience that living with a drug resistant infection does kind of suck.
All of us will have a role to play in this battle. For me, it’s personal. I lost a best friend to a superbug this past December. Lea also had cystic fibrosis, and she died because
Our patient community loved her, respected her and listened to her. In spite of cystic fibrosis, she was a nurse caring for many of the same people you will treat throughout your careers.
Lea has inspired me to prioritize this challenge, and I am hoping to inspire you to face it down in your careers as well. Patients, providers, researchers and drug makers have to come together to develop novel medications and techniques to curtail antimicrobial resistance.
As the challenges you face begin to mount, perhaps you may take some basic advice from the patient standing here today who has stared down one insurmountable challenge after the next.
Don’t be afraid to search outside the box for an answer you may not initially see;
Don’t let the walls of the hospital restrict you from becoming the care provider you have always wanted to be;
and if all else fails, don’t shy away from asking for help.
Feel confident in your decisions and recommendations;
Make eye contact with your patients first and then their family members and support systems;
And above all else, listen. You will be treating people. People who want to feel better and get back to their lives. Some people may not want to play a role in their care, and that is okay! Others will and you need to allow them to do so.
When you are working with a patient, you are offering a recommendation and you must listen to feedback. One of the best things you can do for yourself and the medical outcome of your patient is to learn about the person sitting in the hospital bed. Discover what motivates them, understand the context of their lives and work together to find trust.
You will be challenged, you will continue to learn, and you will succeed in your careers. I look forward to hearing about your accomplishments and how you team up with your future patients.
Feel good about what you are doing, what you have done and what you will do for the care of others so that we may all have the chance to live!
Congratulations to the St. Louis University School of Medicine class of 2019 and welcome to the team!